Nipah virus (NiV) is a rare but grave viral infection that has once again come to public attention following new reported cases in India in early 2026. Often referred to medically as Nipah disease, the WHO has exhibited that this zoonotic virus can spread from animals to humans, and in some cases, from person to person, causing severe respiratory illness and potentially fatal brain inflammation.
What makes Nipah virus especially concerning is its high mortality rate, unpredictable outbreaks, and lack of a widely available vaccine. In recent years, repeated clusters in Kerala established India as a key monitoring region. Now, fresh infections reported from West Bengal have renewed nationwide vigilance, prompting health authorities to strengthen surveillance and public awareness.
Globally, Nipah virus is classified as a priority pathogen due to its epidemic potential and severe outcomes. According to the World Health Organization, fatality rates have ranged from 40% to as high as 75% during past outbreaks, far higher than most common viral infections.
This guide explains Nipah virus in clear, practical terms: what it is, how it spreads, early and severe symptoms, current 2026 outbreak updates in India, available treatment options, vaccine progress, and how to reduce your risk. Whether you’re following the news or simply want accurate information, this pillar page brings together everything you need to know in one place.
This article is for informational purposes only and does not replace professional medical advice.
What Is the Nipah Virus? (2026 Overview)
Nipah virus is a zoonotic virus, meaning it originates in animals and can infect humans. It belongs to the Henipavirus genus and is naturally carried by fruit bats (commonly known as flying foxes). Humans become infected through direct contact with infected animals, contaminated food, or close contact with an infected person.
The virus was first identified during an outbreak in Malaysia in 1998–1999, where it primarily affected pig farmers. Since then, recurring Nipah virus infections have been reported mainly in South and Southeast Asia, with India and Bangladesh experiencing multiple outbreaks over the past two decades.
Once inside the human body, Nipah virus attacks the respiratory system and the central nervous system. Some people experience mild, flu-like illness, while others rapidly develop severe neurological complications such as encephalitis (brain swelling). This wide clinical spectrum, from mild fever to coma, makes early detection challenging.
Another troubling aspect of Nipah infection is its variable incubation period. While symptoms typically appear within 4 to 14 days, medical experts now recognize that, in rare cases, the virus may remain dormant for up to 45 days before symptoms emerge. This “silent period” increases the risk of unnoticed transmission and complicates outbreak control.
Sometimes online searches refer to “Nepo virus” or “Mepa virus.” These are common misspellings — the correct medical term is Nipah virus.
In 2026, Nipah disease remains a major public health concern because there is still no approved antiviral cure, and only experimental vaccines are under clinical trials. As a result, prevention, early symptom recognition, and rapid medical response remain the most effective tools for limiting its impact.
Nipah Virus Symptoms: From Flu-Like Signs to Encephalitis
Nipah virus symptoms can vary widely from person to person. Some infected individuals develop only mild illness, while others progress rapidly to life-threatening neurological complications. This unpredictable pattern is one of the reasons Nipah disease is treated as a medical emergency during outbreaks.
Doctors generally describe Nipah virus symptoms in two stages: early (flu-like) and severe.
Early Symptoms (Usually Days 4–14 After Exposure)
Most cases begin with nonspecific signs that closely resemble common viral infections, which makes early diagnosis difficult. Initial symptoms may include:
- Fever
- Headache
- Muscle pain (myalgia)
- Sore throat
- Fatigue
- Vomiting or nausea
At this stage, many people assume they have seasonal flu or a stomach virus. Because these early Nipah virus symptoms are subtle, infected individuals may continue normal activities, increasing the risk of spreading the virus to others.
Severe Symptoms (Advanced Infection)
In some patients, the infection progresses quickly and begins to affect the brain and lungs. Severe symptoms may include:
- Dizziness or confusion
- Difficulty breathing
- Seizures
- Reduced consciousness
- Acute respiratory distress
- Brain swelling (encephalitis)
Once encephalitis develops, the condition can deteriorate rapidly. Patients may fall into a coma within days, and intensive hospital care becomes critical.
The 45-Day “Silent Period”: Why Nipah Is Hard to Contain
One of the most concerning developments highlighted by medical experts is Nipah’s extended incubation potential.
While most people develop symptoms within 4 to 14 days, rare cases have shown incubation periods lasting up to 45 days. During this silent phase, individuals may feel completely healthy while still carrying the virus.
This delayed symptom onset complicates contact tracing and outbreak control, especially in densely populated areas. It also explains why health authorities closely monitor exposed individuals for several weeks after potential contact.
Skin Rash, Diarrhea, and Less Common Signs
Although respiratory and neurological symptoms dominate, some patients report additional issues such as:
- Diarrhea
- Abdominal discomfort
- Skin rashes or hives
- Persistent cough
These atypical signs sometimes lead people to search online for terms like “nepo virus symptoms” or “stomach virus with rash.” While these are not official medical names, they often reflect confusion caused by Nipah’s wide symptom range.
When to Seek Medical Help
Immediate medical attention is essential if someone experiences fever combined with confusion, breathing difficulty, or seizures, especially in regions reporting Nipah virus outbreaks.
Early hospitalization improves survival chances and helps prevent further transmission.
Current 2026 Nipah Virus Outbreak Status: West Bengal & Kerala
The Nipah virus outbreak in India has entered a new phase in 2026, with recent cases reported in West Bengal alongside continued surveillance in Kerala, two regions that now form the core of the country’s monitoring efforts.
West Bengal: January 2026 Cluster
In early January 2026, health authorities confirmed a small cluster of Nipah virus infections in Barasat, located near Kolkata in West Bengal. The cases triggered rapid response measures, including isolation of suspected patients, contact tracing, and community-level surveillance.
Local hospitals activated infection-control protocols, while public health teams began monitoring individuals who had close contact with confirmed patients. Although the number of reported cases remained limited, the appearance of Nipah virus outside its usual southern hotspots raised concern due to West Bengal’s dense population and high mobility.
Authorities emphasized early testing and public awareness to prevent wider spread, particularly among caregivers and healthcare workers, who face the highest risk during active outbreaks.
Kerala: A Familiar Hotspot
Kerala has experienced multiple Nipah virus outbreaks over the past decade, making it one of India’s most closely watched regions for this disease. Confirmed clusters occurred in:
- 2018
- 2021
- 2023
Each outbreak prompted rapid containment strategies, including quarantine measures, school closures in affected areas, and enhanced hospital preparedness.
Even in 2026, Kerala remains on high alert. Health departments continue routine surveillance, especially in districts with prior infections, and maintain emergency response plans should new cases emerge.
Why India Remains Central to Nipah Monitoring
India’s repeated exposure to Nipah virus is linked to ecological factors such as fruit bat habitats, human population density, and close contact between people and animals. These conditions increase the likelihood of spillover events, where the virus jumps from bats to humans.
Because of this pattern, Nipah virus in India often spikes during outbreak periods, reflecting widespread public concern and the need for reliable information.
Globally, Nipah is classified as a priority pathogen due to its epidemic potential, high fatality rate, and lack of approved vaccines. Every new cluster, whether in Kerala, West Bengal, or neighboring countries, is treated as a serious public health event.
How Nipah Virus Spreads
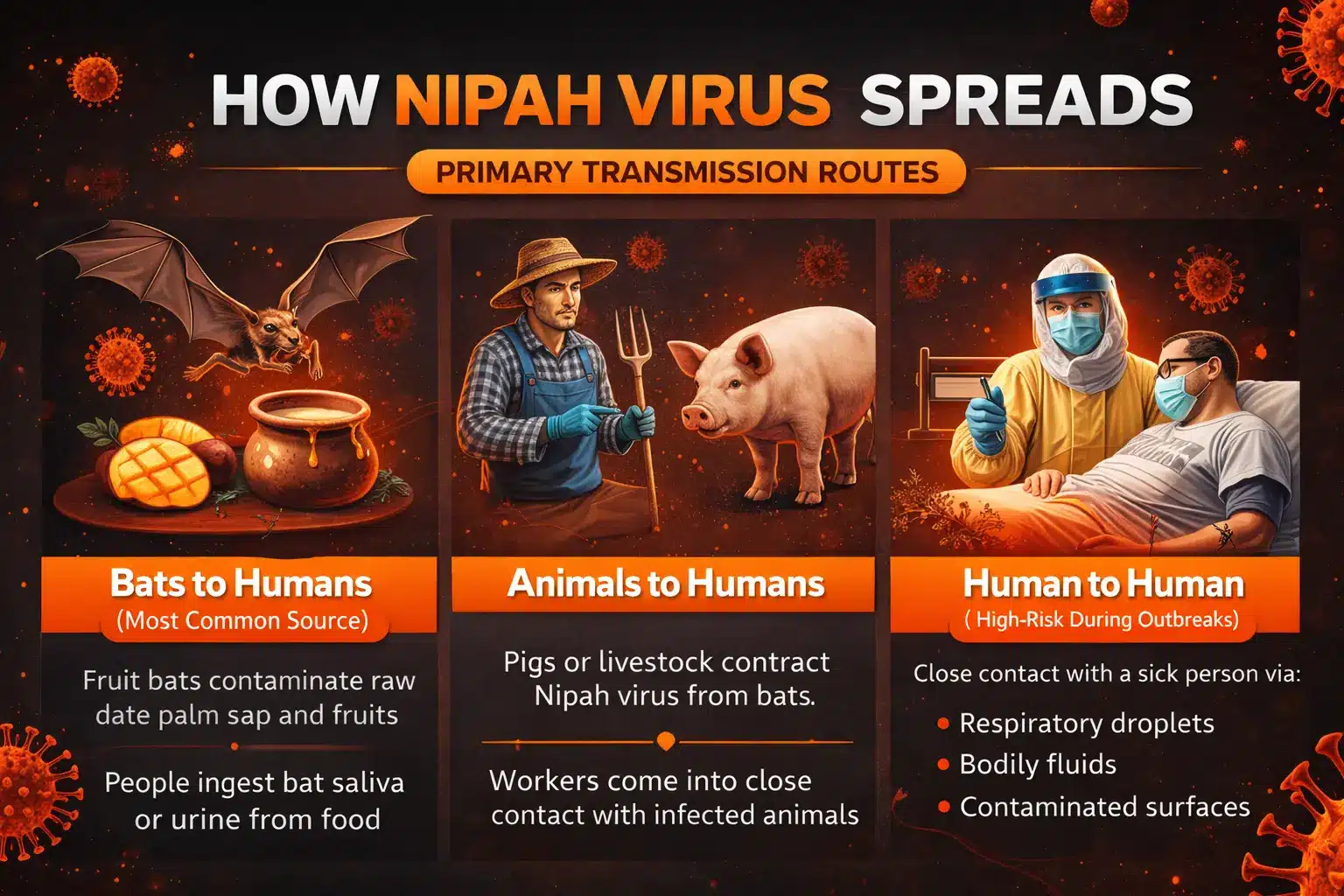
Understanding how Nipah virus spreads is critical for preventing infection, especially during active outbreaks. Unlike many common viruses, Nipah transmission involves both animals and humans, making control more complex.
Health experts recognize three primary transmission routes:
1. From Bats to Humans (Most Common Source)
Fruit bats (flying foxes of the Pteropus species) are the natural carriers of Nipah virus, and bat-to-human spillover is the most common way outbreaks begin. Humans typically become infected after consuming food contaminated with bat saliva, urine, or feces, especially raw date palm sap collected overnight in open containers that attract bats.
Epidemiological investigations in South Asia show how significant this route is: during Bangladeshi outbreaks, about 64% of Nipah patients reported drinking raw date palm sap, compared with only 18% of uninfected individuals, making sap consumption one of the strongest documented risk factors. Most primary cases also occur during the sap harvesting season (December to March), when bats frequently lick collection pots or urinate into exposed sap.
Partially eaten fruits can also transmit the virus if consumed without proper washing or peeling. While domestic animals such as pigs have acted as intermediate hosts in some outbreaks, contaminated food from bats remains the primary trigger for human Nipah infections across South Asia, which is why avoiding raw sap and practicing food hygiene are critical prevention measures.
2. From Animals to Humans
In some cases, domestic animals act as intermediate hosts. Pigs were involved in the original Malaysian outbreak, and other livestock may potentially transmit the virus after exposure to bats.
People working closely with animals, farmers, handlers, or slaughterhouse workers face a higher risk if proper hygiene and protective measures are not followed.
3. Human-to-Human Transmission (High-Risk During Outbreaks)
Nipah virus can also spread directly between people through close contact with:
- Respiratory droplets
- Bodily fluids (saliva, urine, blood)
- Contaminated surfaces
This route is especially dangerous in hospitals and households, where caregivers and healthcare workers may be exposed while treating infected patients.
Unlike airborne viruses such as measles, Nipah does not spread freely through the air over long distances. Transmission usually requires close, prolonged contact, which is why isolation and protective equipment are so important once a case is identified.
Why Transmission Control Is Challenging
Two factors make Nipah particularly difficult to contain:
- Early symptoms resemble common flu, delaying diagnosis
- The incubation period can extend up to 45 days in rare cases
This means people may unknowingly spread the virus before realizing they are infected.
For this reason, outbreak response focuses heavily on rapid testing, contact tracing, and strict infection prevention measures in healthcare settings.
Is There a Nipah Virus Vaccine?
Vaccine Development: A Major 2026 Breakthrough
The Coalition for Epidemic Preparedness Innovations (CEPI) reports that the University of Oxford has launched the world’s first Phase II Nipah virus vaccine trial in Bangladesh. Nipah is listed by the World Health Organization as a priority pathogen due to its pandemic potential and fatality rates of up to 75%.
The vaccine candidate (known as ChAdOx1 NipahB) is currently being tested for safety and immune response in human volunteers, primarily in South Asia. While results are still pending, this marks the most advanced Nipah vaccine effort to date.
Global health agencies such as the World Health Organization classify Nipah as a priority pathogen — meaning vaccine development is being fast-tracked compared to many other emerging viruses.
That said, even under optimistic timelines, widespread public availability is still likely years away.
How Is Nipah Virus Treated Right Now?
Because there is no approved cure, current Nipah virus treatment focuses on intensive supportive care, which may include:
- Oxygen therapy or ventilator support
- IV fluids and electrolyte management
- Medications to control seizures
- Treatment of secondary infections
- Continuous neurological monitoring
Patients with severe disease are typically managed in intensive care units.
In limited experimental settings, doctors have also used monoclonal antibodies and antiviral drugs under compassionate-use protocols. These treatments are still under study and are not considered standard care.
How to Test for Nipah Virus Infection
Testing for Nipah virus is done only in specialized laboratories, usually after a doctor identifies symptoms and possible exposure during an outbreak.
Diagnosis typically involves collecting samples such as:
- Throat or nasal swabs
- Blood
- Urine
- Cerebrospinal fluid (in severe neurological cases)
The most common tests include:
- RT-PCR (Reverse Transcriptase Polymerase Chain Reaction), detects the virus’s genetic material in the early stage of infection
- ELISA blood tests identify antibodies after the immune system responds
Because Nipah virus is highly contagious and dangerous, samples are handled under strict biosafety conditions, and results may take time depending on laboratory capacity.
Doctors usually recommend testing if someone has:
- Fever plus neurological or breathing symptoms
- Recent contact with a confirmed case
- Exposure in an active outbreak area
Early testing helps guide isolation decisions and supportive treatment — both critical for preventing further spread.
Prevention Tips During a Nipah Virus Outbreak
Because there is no approved vaccine yet, prevention remains the most effective defense against Nipah virus, especially in regions reporting active cases.
Health authorities recommend the following measures to reduce infection risk:
Personal Safety
- Avoid drinking raw date palm sap or fresh juice sold openly
- Do not eat fruits that appear bitten or damaged by animals
- Always wash, peel, or cook fruits before consumption
- Practice frequent handwashing with soap and water
- Avoid close contact with anyone showing fever or respiratory symptoms
Caregiver & Healthcare Precautions
People caring for suspected or confirmed Nipah patients should:
- Wear gloves and masks when in close contact
- Avoid direct exposure to bodily fluids
- Disinfect commonly touched surfaces regularly
- Follow strict isolation and hygiene protocols
Healthcare workers are advised to use full Infection Prevention and Control (IPC) measures, including protective clothing and controlled patient handling.
Travel Awareness
If traveling to outbreak-affected areas:
- Monitor your health for at least 2–3 weeks after return
- Seek medical advice immediately if symptoms appear
- Inform doctors about recent travel history
Simple habits — hygiene, food safety, and early medical consultation — play a powerful role in stopping Nipah virus transmission before it spreads further.
Frequently Asked Questions
Can Nipah virus spread through the air?
Nipah virus does not spread freely through the air like measles. Transmission usually happens through close contact with respiratory droplets or bodily fluids from an infected person. This means prolonged face-to-face interaction, caregiving, or medical procedures pose the highest risk. Proper isolation and protective equipment significantly reduce transmission.
Is Nipah virus the same as COVID-19?
No. Nipah virus and COVID-19 are caused by completely different viruses and behave very differently.
COVID-19 spreads easily through aerosols and has a much lower fatality rate. Nipah virus spreads mainly through close contact but carries a far higher risk of severe neurological disease and death. Nipah outbreaks tend to be smaller, but much more dangerous per case.
How long should someone be monitored after exposure?
Most people develop symptoms within 4–14 days, but rare cases have shown incubation periods of up to 45 days. For this reason, exposed individuals are often monitored for several weeks during outbreaks.
Conclusion
Nipah virus remains one of the world’s most dangerous emerging infections, not because it spreads easily, but because of how severe it becomes once it does. With fatality rates far higher than most viral illnesses, unpredictable incubation periods, and no approved vaccine yet, even small outbreaks demand serious attention.
The 2026 cases in West Bengal, alongside Kerala’s history of repeated clusters, highlight why India continues to be closely monitored for Nipah disease. While promising vaccine trials are underway, prevention, early symptom recognition, rapid testing, and supportive hospital care remain the strongest tools available today.
Simple actions, such as avoiding contaminated food, practicing good hygiene, seeking medical help early, and following public health guidance, can make a real difference in limiting the spread and saving lives.
Staying informed is not about fear. It’s about readiness.